Opinion Piece: Ashwin Swaminathan is a Senior Lecturer at the College of Health and Medicine at the Australian National University
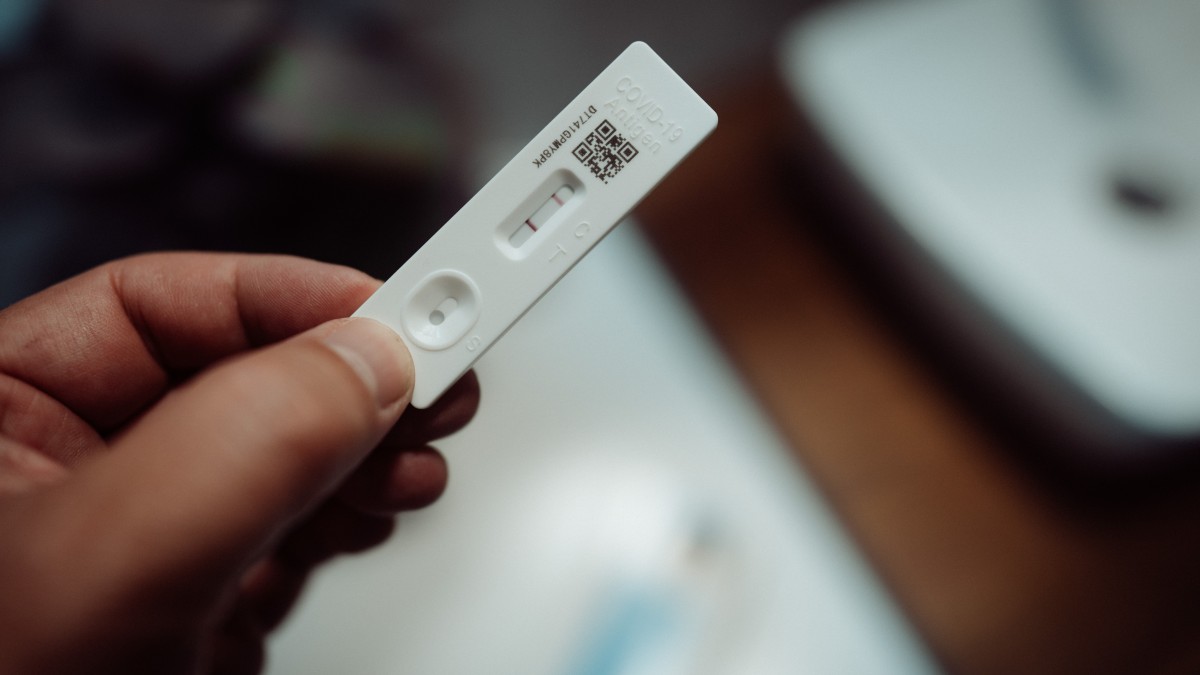
As Omicron surges through the community, getting the right answer from a Rapid Antigen Test (RAT) is not as straightforward as reading one or two lines off the kit.
RATs are a convenient diagnostic tool to detect COVID virus fragments in nasal secretions or saliva. They are designed to be self-administered and give an answer in minutes. Detecting infection early is critical to preventing spread and allowing persons at risk of severe disease to get timely access to close monitoring and new life-saving therapies.
As governments plan to distribute tens of millions of RAT kits to schools and workplaces in coming weeks to help Australians work and study safely, it is important that we understand how to best use this diagnostic tool to reduce transmission and unnecessary disruptions to our lives and economy.
Key concepts
There are three key concepts to understanding how accurate RATs (or any diagnostic test) are: sensitivity, specificity and pre-test probability.
Let’s imagine we line up 100 people who definitely have COVID infections. Applying a RAT kit with 80% sensitivity would lead to a positive result in 80 people – with 20 receiving a “false negative” result. So the term “sensitivity” refers to how well a test picks up the presence of a disease or condition.
If we line up 100 people who are definitely free of COVID infection, using a RAT test with 98% specificity would mean that 98 would test negative – and two people would have a “false positive”. So “specificity” is whether a test correctly identifies the absence of a disease or condition.
The “pre-test probability” of infection is the likelihood a person has COVID infection based on their clinical symptoms, exposure history and/or the background community rate of infection. The pre-test probability (otherwise known as “disease prevalence”) varies between households, workplaces and communities and provides context to a RAT kits sensitivity and specificity.
3 people, 3 tests
Let’s look at how we can apply the above concepts to three typical Australian scenarios. Let’s assume a TGA-approved self-test RAT kit with a minimum sensitivity of 80% and specificity of 98% was used. Probability calculations are performed using an online tool.
These scenarios are not intended as medical advice but as illustrations of key concepts only.
1. Ahmed is a 48 year-old office worker, double vaccinated and booked in for a booster shot
He lives in a household of four with two COVID-positive teenagers. He has developed a fever and sore throat. He has undertaken a RAT and has a positive result. What should he do next?
The pre-test probability of COVID for Ahmed is high (at least 80% – an educated estimate based on risk factors) given he is a household close contact, has developed typical symptoms and has not been boosted. In this situation, a positive RAT result is >99% likely to represent true infection. The best thing Ahmed can do is register the positive result, rest up, keep up his fluids, take paracetamol if required and quarantine for at least seven days.
2. Kim is 15 years old and lives in a capital city with her family
She recently received her second vaccination. She does not have COVID symptoms and has no known contacts. She self-tests with a RAT kit distributed by her school and returns a positive test. What does this mean?
The pre-test probability of COVID in Kim is low given her recent vaccination, lack of symptoms or exposure history. The current population rate of COVID in Canberra is around 2% based on reported cases and factoring in likely under-reporting. This prevalence is likely similar to that in Sydney or Melbourne. So Kim’s positive RAT result would only be 50% likely to represent true infection. In this instance, Kim should confirm the result by getting a PCR test. She should quarantine until she receives that result but a negative PCR result might mean she and her family avoid unnecessary isolation.
3. Margaret is a 63 year-old disability support worker who has received a booster vaccination
She is on medication for arthritis that affects her immune system. Three days ago, while intermittently wearing a surgical mask, she cared for a man in his home for six hours. He was later diagnosed with COVID. Margaret is asymptomatic and self-tests with a RAT kit that returns a negative result. What should she do?
Margaret’s pre-test probability of COVID is estimated to be moderate to high (~50%) given she was a close contact, had inadequate mask protection and her medication may reduce vaccine protection. A negative result is 83% likely to be accurate. Margaret should err on the side of caution by isolating then repeating the RAT 48 hours later. As it happens, she has developed a cough and runny nose within that time and returns a positive test.
How else can I improve my RAT accuracy?
The accuracy of RATs can be affected by factors such as how well the sample is taken, the timing of the sample (RATs are relatively insensitive early or late in infection) and the evidence particular brands have differing ability to detect the Omicron variant. The TGA is currently reviewing and reporting the evidence provided for kits on sale and how sensitive they are to specific COVID variants.
So, to get the most out of your RAT, do the following:
- follow the kit instructions closely
- time your test – don’t perform within 48 hours of exposure to COVID and preferably wait or repeat between 5–7 days post exposure
- if your test result is a surprise based on your assessment of pre-test probability (you think there is a good chance of a false positive or negative result), then take appropriate precautions and repeat the test 24–48 hours later or have a PCR test done.
Ashwin Swaminathan is a Senior Lecturer at the ANU College of Health and Medicine. Article first published in The Conversation: How accurate is your RAT? 3 scenarios show it's about more than looking for lines (theconversation.com)